![]()
![]()
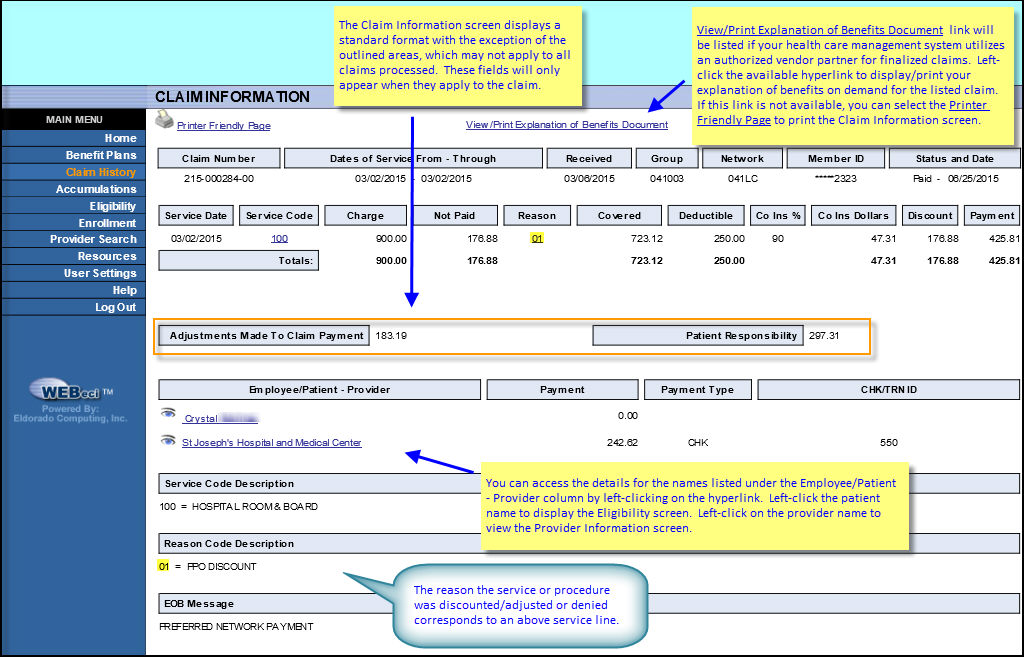
Fields |
Definitions |
Claim Number |
A system assigned number used to identify a claim. The first three digits refer to the year (218 = 2018). The next six digits identify the claim. The last two digits may have multiple meanings: |
Dates of Service From-Through |
The first and last dates that services were performed for this claim. |
| Received | The date that the claim was received for processing. |
Group |
All patients are associated with a group - this is typically an employer, but can also be a division or sub-division within the employer. Each group is identified by a unique code which is what you see here. |
Network |
Identifies the network through which the service was provided and applicable benefits were assessed. |
Member ID |
The system-assigned code used to identify the patient in lieu of a social security code, per HIPAA requirements. |
Status and Date |
The current status of the claim, and the date this status went into effect. Status options are: |
Service Date |
The date the service was performed. |
Service Code |
Three-character code for a specific service. |
Charge |
The amount charged / billed for the specific service or procedure. |
Not Paid |
The total amount of the charge that is not covered under the benefit plan. |
Reason |
This two-character code represents the reason that the claimed service or procedure charge was adjusted or denied. |
Covered Amount |
The total covered amount for the claim. This is the amount of the claim that your insurance will pay. |
Deductible |
Lists the base, dollar-denominated amount that a patient is required to payout-of-pocket toward the charges incurred. |
Co Ins % |
The percentage of the service charge that your insurance covers. |
Co Ins Dollars |
The dollar amount that your insurance covers for the listed service. |
Discount |
Lists the dollar-denominated amount that the provider has agreed to waive for the claimed service(s). |
Payment |
The amount paid to the patient or provider before adjustments. |
Totals |
Lists the total charges, total not-paid amounts, total covered amounts, total deductible amounts, total coinsurance dollars and total payments, in that order, for the preceding service lines of the claim. |
Adjustments Made To Claim Payments |
The total amount of calculated adjustments. |
Patient Responsibility |
The amount that the patient is responsible for paying. |
Employee/Patient - Provider |
Lists the patients and/or providers attached to this claim. Underlined provider names appearing in blue are hyperlinks. Left-click on the name to view provider address and contact information. |
Withhold |
PPO providers can have withholds done when claims are processed and paid. A portion of the payment amount, per service line, can be withheld according to the option that the provider has selected, either a percentage per line or a flat amount per line. These amounts are not paid to the provider at the time of the claim payment, but can be recouped at the end of the year. |
Encountered |
Encountered is when there is a “capitated” dollar amount taken during the pricing of the claim. This is a negotiated amount for one or more services covered by a capitation agreement and is deducted from the provider’s claim payment. |
Payment |
If a payment has been paid towards this claim, the amount paid will be shown. If this field is blank, a payment has not been made. |
Check Number |
If a payment has been paid towards this claim, the check number used will be shown. If the claim number field is blank, no payment has been made. |
Service Code Description |
A short description of the service code(s) used in the Service Code column, above. For more information, contact your Benefit Administrator. |
Reason Code Description |
A short description of the reason codes used in the Reason Code column. |