![]()
![]()
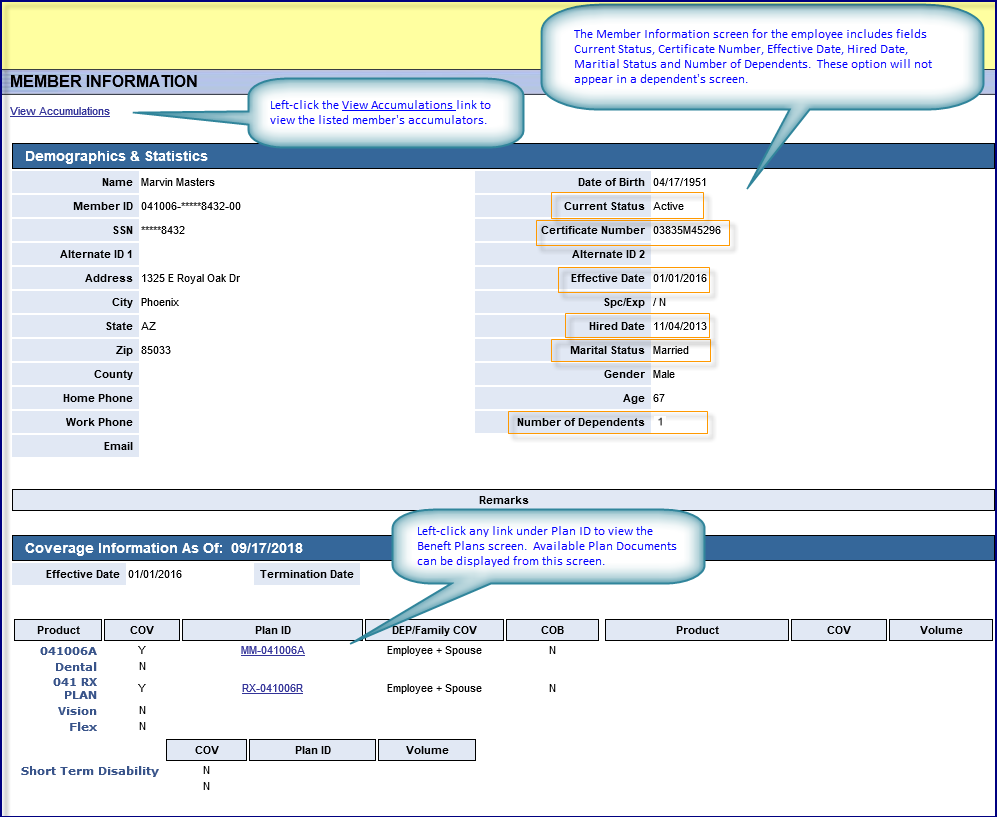
The Demographics & Statistics screen lists the member's basic demographic (i.e., personal) information, user remarks, coverage information and provides links to the member's benefit accumulator history and benefit plans.
Fields |
Definitions |
|
|
View Accumulations hyperlink
|
Left-click to open the insured's Accumulations screen. |
|
|
Demographics & Statistics
|
Definitions are only provided for those fields whose meaning isn't self-explanatory. |
|
|
Name
|
First name Last Name format |
Date of Birth
|
Indicates the member's date of birth. |
Member ID
|
Identifies the member by combining the member's:
Format: UUUGGG-123456789-00
|
Current Status
|
Indicates the patient's current coverage status. |
SSN
|
Indicates the member's social security number. |
Certificate Number
|
Indicates the HP4-specific, internal ID assigned to the member. |
Alternate ID 1
|
Each member record now includes Alternate ID 1 and Alternate ID 2 fields. Once an alternate ID has been created for the member, you can use it to search for the member's record instead of the Member ID. Up 20 alphanumeric characters are allowed, including hyphens. It doesn't include spaces.
|
Alternate ID 2
|
See preceding description.
|
Address
|
Indicates the member's street address or PO Box.
|
Effective Date
|
This is the member's initial effective date. For example, If the employee is terminated and later rehired, the first effective date reflects the first coverage effective date following the rehiring.
|
City
|
Indicates the List(s) the name of the municipality that the employee is located in.
|
Spc/Exp
|
|
State
|
List(s) the state postal code of the member.
|
Hired Date
|
Indicates the member's official date of hiring. The hire date is instrumental in defining eligibility dates and may be used when creating HIPAA certificates.
|
Zip
|
Indicates the ZIP code of the member's address. |
Marital Status
|
Options are: Married or Single.
|
County
|
Indicates the name of the county that the member is located in. |
Gender
|
Indicates the member's gender. |
Home Phone
|
Indicates the member's primary contact number at home (or away from the member's place of employment). |
Age
|
Indicates the member's age based on the listed date of birth |
Work Phone
|
Indicates the member's primary contact number at a place of employment (or away from the member's home).
|
Number of Dependents
|
Indicates the total number of employee dependents. |
|
Indicates the member's preferred email address, if available. |
|
|
Remarks
|
Remarks are user-defined in HEALTHpac.
|
|
|
Coverage Information As Of
|
|
|
|
Effective Date
|
This is the member's initial effective date. For example, If the employee is terminated and later rehired, the first effective date reflects the first coverage effective date following the rehiring.
|
Termination Date
|
Indicates the employee’s termination date or effective date of COBRA coverage from the Employee Master Eligibility record, if applicable.
|
Product
|
Lists system standard products.
|
COV
|
Indicates whether the adjacent coverage is currently in force using either a (Y)es or a (N)o.
|
Plan ID
|
Each of the options shown in the Plan ID column are also hyperlinks. Left-click the desired option to view the corresponding Benefit Plans screen (live link) for the listed member.
|
DEP/Family COV
|
Indicates the applicable coverage type for the adjacent product. |
COB
|
Indicates whether coordination of benefits applies to the listed member. |
Product
|
Lists supplemental products selected by the group, if applicable.
|
COV
|
Indicates whether the adjacent supplemental product was also selected by the member, if applicable, and is in force using either a (Y)es or a (N)o.
|
Volume
|
Indicates the applicable volume of coverage (e.g., 10000 = $10,000 of coverage). |